Atorvastatin is a member of the medication class known as statins, which are used primarily as a lipid-lowering agent and for prevention of events associated with cardiovascular disease. Like all statins, atorvastatin works by inhibiting HMG-CoA reductase, an enzyme found in liver tissue that plays a key role in production of cholesterol in the body.
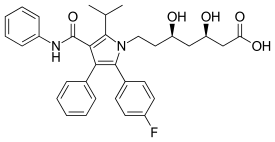
Molecular Structure |
Class of Drug |
Antilipidemic agent.
Mechanism of Action |
Inhibits HMG-CoA reductase. Reduces total LDL, cholesterol, serum triglyceride levels. There is little if any effect on serum HDL levels
Indications / Dosage / Route |
Routes of Administration: Oral only
Condition: Hyperlipidemia
Dose: Adults Initial: 10 mg/d. Maintenance: 10-80 mg/d.
Condition: Homozygous familial hypercholesterolemia
Dose: Adults 10-80 mg/d.
Adjustment of Dosage |
Kidney disease: None.
Liver disease: None.
Elderly: None
Pediatric: Limited data available.
Food and Drug Interactions |
Food: No restriction.
Pregnancy: Category X—contraindicated.
Lactation: Appears in breast milk. Contraindicated.
Contraindications: Hypersensitivity to statins, active liver disease or unexplained persistent elevations of serum transaminase, pregnancy, lactation.
Warnings / Precautions |
> Use with caution in patients with the following conditions: renal insufficiency, history of liver disease, alcohol abusers.
> Discontinue if drug-induced myopathy develops. This is characterized by myalgia, creatinine kinase levels >10x normal. May cause acute renal failure from rhabdomyolysis. May occur more frequently when drug is combined with gemfibrozil or niacin.
> Discontinue drug if patient experiences severe trauma, surgery, or serious illness.
Clinically Important Drug Interactions |
> Drugs that increase effects/toxicity of HMG-CoA reductase inhibitors: gemfibrozil, clofibrate, erythromycin, cyclosporin, niacin, clarithromycin, itraconazole, protease inhibitors.
> HMG-CoA reductase inhibitors increase effects/toxicity of oral anticoagulants.
Adverse Reactions |
> Common: None.
> Serious: myopathy, rhabdomyolysis, neuropathy, cranial nerve abnormalities, hypersensitivity reactions, pancreatitis, hepatic injury including hepatic necrosis and cirrhosis, lens opacities
Parameters to Monitor |
> Total cholesterol, LDL and HDL cholesterol, triglycerides. Values should be obtained prior to and periodically after treatment begins to ascertain drug efficacy.
> Serum BUN and creatinine.
> Monitor liver enzymes before beginning therapy, at 3, 6, and 12 months thereafter, and semiannually afterward.
> Signs and symptoms of myopathy: unexplained skeletal muscle pain, muscle tenderness or weakness particularly when accompanied by fever or fatigue. Check creatinine kinase levels. If these are markedly elevated or patient is sympto-matic, discontinue drug.
> Discontinue drug if transaminase levels exceed three times normal values. It may be advisable to take a liver biopsy if transaminase elevation persists after drug is discontinued.
> Patient’s ophthalmic state should be evaluated once a year following treatment. If lens opacity occurs, consider discontinuing drug.
Advice to Patient |
> Avoid alcohol.
> Use of OTC medications only with approval from treating physician.
> Exercise regularly, reduce fat and alcohol intake, and stop smoking.
Further Useful Info |
> Current literature suggests that the most effective reduction of total and LDL cholesterol occurs with a combination of exercise, weight reduction, low-fat diet, and lipid-lowering agents.


