Amlodipine is a medication used to treat high blood pressure and coronary artery disease. While not typically recommended in heart failure, amlodipine may be used if other medications are not sufficient for high blood pressure or heart-related chest pain. Amlodipine is taken by mouth and has an effect for at least a day.
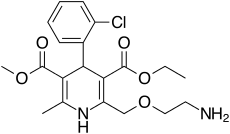
Molecular Structure |
Class of Drug |
Calcium channel blocker.
Mechanism of Action |
Inhibits calcium movement across cell membranes.
Indications / Dosage / Route |
Routes of Administration: Oral only.
Condition: Hypertension
Dose: Adults Individualize: 2.5-5 mg/d. Maximum: 10 mg/d.
Condition: Angina
Dose: Adults 5-10 mg.
Elderly – 5 mg
Adjustment of Dosage |
Kidney disease: Use with caution.
Liver disease: Initial dose 2.5 mg/d.
Elderly: Initial dose 2.5 mg/d.
Pediatric: Safety and efficacy have not been established in children
| Onset of Action | Peak Effect | Duration |
| 1-2 h | 6-12 h | 24 h |
Food and Drug Interactions |
Food: No restriction.
Pregnancy: Category C.
Lactation: Probably appears in breast milk. Potentially toxic to infant. Avoid breastfeeding.
Contraindications: Hypersensitivity to calcium blockers.
Warnings / Precautions |
> Use with caution in patients with the following conditions: CHF, severe left ventricular dysfunction, concomitant use with β blockers or digoxin.
> Do not withdraw drug abruptly, since this may result in increased frequency and intensity of angina.
> For the diabetic patient, amlodipine may interfere with insulin release and therefore produce hyperglycemia.
> Patient should be tapered off P blockers before beginning cal-cium channel blockers to avoid exacerbation of angina due to abrupt withdrawal of the β blocker.
Clinically Important Drug Interactions |
> Drugs that increase effects/toxicity of calcium blockers: cimetidine, β-blockers, cyclosporine.
> Drugs that decrease effects of calcium blockers: barbiturates.
Adverse Reactions |
> Common: headache, edema.
> Serious: CHF, arrhythmias, hypotension, depression.
Parameters to Monitor |
> Patient’s BP during initial administration and frequently thereafter. Ideally, check BP close to the end of dosage interval or before next administration.
> Status of liver and kidney function. Impaired renal function prolongs duration of action and increases tendency for toxicity.
> Intake of fluids and urinary and other fluid output to minimize renal toxicity. Increase fluid intake if inadequate. Closely monitor electrolyte levels.
Advice to Patient |
> Use two forms of birth control including hormonal and barrier methods.
> Change position slowly, in particular from recumbent to upright, to minimize orthostatic hypotension. Sit at the edge of the bed for several minutes before standing, and lie down if feeling faint or dizzy. Avoid hot showers or baths and standing for long periods. Male patients should sit on the toilet while urinating rather than standing.
> Avoid driving and other activities requiring mental alertness or that are potentially dangerous until response to drug is known.
> Avoid use of OTC medications without first informing the treating physician.
> Determine blood pressure and heart rate aproximately at the same time each day and at least twice a week, particularly at the beginning of therapy.
> Be aware of the fact that this drug may also block or reduce anginal pain, thereby giving a false sense of security on severe exertion.
> Include high-fiber foods to minimize constipation.
> Limit consumption of xanthine-containing drinks: regular coffee (fewer than 5 cups/day), tea, cocoa.


