Amitriptyline is a medicine primarily used to treat a number of mental illnesses. These include major depressive disorder and anxiety disorders, and less commonly attention deficit hyperactivity disorder and bipolar disorder. Other uses include prevention of migraines, treatment of neuropathic pain such as fibromyalgia and postherpetic neuralgia, and less commonly insomnia. It is in the tricyclic antidepressant (TCA) class and its exact mechanism of action is unclear. Amitriptyline is taken by mouth.
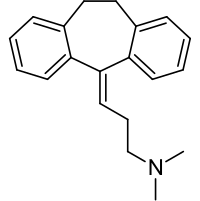
Molecular Structure |
Class of Drug |
Tricyclic Antidepressant.
Mechanism of Action |
Inhibits reuptake of CNS neurotransmitters, primarily serotonin and norepinephrine
Indications / Dosage / Route |
Routes of Administration: Oral and IM.
Condition: Depression
Dose: Adults – Out-patients: Initial: PO 75 mg/d in divided doses; increase to 150 mg/d if needed.
Hospitalized Patients: PO Initial: 100 mg/d, may be increased to 200-300 mg/d. IM 20-30 mg q.i.d.; change to oral drug as quickly as possible. Maintenance: 40-100 mg/d.
Adolescents and elderly: PO 10 mg t.i.d. with 20 mg at bed-time. Maximum: 100 mg/d.
Children 6-12 years: PO 10-30 mg/d, up to 4 divided doses.
Condition: Chronic pain
Dose: Adults PO 50-100 mg/d.
Condition: Enuresis
Dose: Children >6 years: PO 10 mg/day at bedtime; increase to maximum of 25 mg/day if needed.
Children <6 years: PO 10 mg/day at bedtime.
Adjustment of Dosage |
Kidney disease: None.
Liver disease: None.
Elderly: See above.
Pediatric: Not recommended for children < 12 years old except for treatment of enuresis.
Food and Drug Interactions |
Food: No restriction.
Pregnancy: Category C.
Lactation: Appears in breast milk. American Academy of Pediatrics expresses concern over use when breastfeeding.
Contraindications: Hypersensitivity to tricyclic antidepressants, acute recovery from MI, concurrent MAO inhibitor
Warnings / Precautions |
> Use with caution in patients with the following conditions: epilepsy, angle-closure glaucoma, cardiovascular disease, his-tory of urinary retention, suicidal tendencies, benign prostatic hypertrophy, concurrent anticholinergic drugs, hyperthyroid patients receiving thyroid drugs, alcoholism, schizophrenia.
> May cause psychosis in schizophrenic patients.
> May unmask mania or hypomania.
Clinically Important Drug Interactions |
> Drugs that increase effects/toxicity of tricyclic antidepressants: MAO inhibitors, cimetidine, SSRIs, β-blockers, estrogens.
> Drugs that decrease effects/toxicity of tricyclic antidepres-sants: barbiturates, cholestyramine.
> Tricyclic antidepressants increase effects/toxicity of following drugs: CNS depressants (alcohol, sedatives, hypnotics), oral anticoagulants, carbamazepine, sympathomimetic amines (dobutamine, dopamine, epinephrine, ephedrine), opioids (morphine-type drugs), drugs with anticholinergic activity (atropine, anti-Parkinson drugs).
> Tricyclic antidepressants decrease effects/toxicity of following drugs: clonidine, guanethidine.
Adverse Reactions |
> Common: sedation, anticholinergic effects (dry mouth, constipation), nausea, dizziness, headache, taste disturbance, weight gain.
> Serious: orthostatic hypotension, arrhythmias, extrapyramidal symptoms, seizures, bone marrow depression, hepatitis, increased intraocular pressure, allergic reactions.
Parameters to Monitor |
> CBC with differential and platelets, liver enzymes.
Advice to Patient |
> Avoid alcohol and other CNS depressants such as opiate analgesics and sedatives (eg, diazepam) when taking this drug.
> Avoid driving and other activities requiring mental alertness or that are potentially dangerous until response to drug is known.
> Change position slowly, in particular from recumbent to upright, to minimize orthostatic hypotension. Sit at the edge of the bed for several minutes before standing, and lie down if feeling faint or dizzy. Avoid hot showers or baths and standing for long periods. Male patients should sit on the toilet while urinating rather than standing.
> If mouth is dry rinse with warm water frequently, chew sugarless gum, suck on ice cube, or use artificial saliva. Carry out meticulous oral hygiene (floss teeth daily).
> To minimize possible photosensitivity reaction, apply adequate sunscreen and use proper covering when exposed to strong sunlight.
> If constipation develops, increase fiber and fluid intake. Notify physician if constipation is severe.


