Ranitidine is a medication which decreases stomach acid production. It is commonly used in treatment of peptic ulcer disease, gastroesophageal reflux disease, and Zollinger Ellison syndrome. There is also tentative evidence of benefit for hives
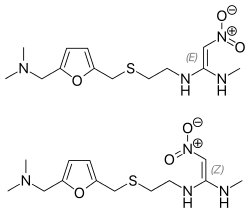
Molecular Structure |
Class of Drug |
H2 receptor blocker.
Mechanism of Action |
Competitively blocks H2 receptors on parietal cells, thereby blocking gastric acid secretion.
Indications / Dosage / Route |
Routes of Administration: Oral, IV and IM.
Condition: Duodenal ulcer, short-term
Dose: Adults: PO150 mg b.i.d. or 300 mg h.s.
Maintenance: 150 mg h.s.
Condition: Pathologic hypersecretory conditions
Dose: Adults: 150 mg b.i.d. Maximum: 6 g/d.
Condition: Benign gastric ulcer
Dose: Adults: 150 mg b.i.d.
Maintenance: 150 mg h.s.
Condition: GERD
Dose: Adults 150 mg b.i.d.
Condition: Erosive esophagitis
Dose: Adults 150 mg q.i.d. Maintenance of healing of erosive esophagitis
Condition: Duodenal ulcer, hypersecretory conditions, GERD
Dose: Adults: IM 50 mg q6-8h. Intermittent IV injection or infusion: 50 mg q6-8h
Maximum: 400 mg/d. Continuous IV infusion: 6.25 mg/h.
Condition: Zollinger-Ellison syndrome
Dose: ©Continuous IV infusion: 1-2.5 mg/kg/h may be necessary
Adjustment of Dosage |
Kidney disease: None
Liver disease: None.
Elderly: None
Pediatric: Safety and efficacy have not been established.
| Onset of Action | Peak Effect | Duration | |
| Oral | — | 1-3 h | 13 h |
Food and Drug Interactions |
Food: Take with food.
Pregnancy: Category B.
Lactation: Appears in breast milk. Cimetidine (another H2 blocker) is considered compatible by American Academy of Pediatrics.
Contraindications: Hypersensitivity to H2 blockers.
Warnings / Precautions |
> Use with caution in the elderly, in patients with hepatic or liver disease, and in immunocompromised patients.
> Symptomatic rehef does not mean absence of gastric malignancy.
> Adverse reactions are most likely to occur in elderly and in patients who have impaired renal function.
> Avoid driving and other activities requiring mental alertness or that are potentially dangerous until response to drug is known.
> Discontinue drug for 24-72 hours before performing skin test for allergens.
> Decreased gastric acidity may increase the possibility of intes-tinal parasites and bacterial overgrowth, particularly in immuno compromised patients.
Clinically Important Drug Interactions |
> None.
Adverse Reactions |
> Common: None.
> Serious: Arrythmias, jaundice, bone marrow suppression, aplastic anemia (rare), hypersensitivity reactions.
Parameters to Monitor |
> Efficacy of treatment: improved symptoms of gastroesoph ageal reflux or peptic ulcer disease.
> Presence of Helicobacter pylori. This is a standard approach in patients with peptic ulcer disease.
> Use endoscopy to prove healing of gastric ulcers. A nonhealing gastric ulcer may actually be due to gastric cancer.
> Symptoms of serious underlying disease requiring further testing (weight loss, worsening abdominal pain, early satiety, etc).
Advice to Patient |
> Avoid alcohol and smoking.
> Avoid caffeine and foods that might cause GERD.
> Continue taking drug even after reduction in ulcer pain.
> Report ongoing use of OTC H2 blockers to your physician.
Further Useful Info |
> Current management of peptic ulcer disease uses diagnosis and treatment of II. pylori infection. Check if patients are receiving NSAIDs and discontinue when possible. Hypersecretory states are uncommon causes of peptic ulcer disease.
> H2 blockers are the drugs of choice for the following conditions: dyspepsia not evaluated by endoscopy (empirical), mild to moderate GERD, peptic ulcer disease not due to H. pylori infection.
> Proton pump inhibitors are essentially replacing H2 blockers for management of GERD.


