Metoprolol is a medication of the selective β1 receptor blocker type. It is used to treat high blood pressure, chest pain due to poor blood flow to the heart, and a number of conditions involving an abnormally fast heart rate. It is also used to prevent further heart problems after myocardial infarction and to prevent headaches in those with migraines.
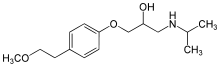
Molecular Structure |
Class of Drug |
β-Adrenergic receptor blocker
Mechanism of Action |
Competitive blocker of β-adrenergic receptors in heart and blood vessels.
Indications / Dosage / Route |
Routes of Administration: Oral and IV.
Condition: Angina pectoris
Dose: Adults: PO 100 mg/d in a single dose. Increase at weekly intervals until optimum effect is reached. Maximum: 400 mg/d.
Condition: Hypertension
Dose: Adults: PO 50-100 mg/d in a single dose with or without a diuretic. Increase weekly until maximum effect is achieved. Maximum: 400 mg/d.
Condition: Prophylaxis of migraine
Dose: PO 50-100 mg b.i.d.
Condition: Ventricular arrhythmias
Dose: PO 200 mg/d.
Condition: Early treatment of MI
Dose: 3 IV bolus injections of 5 mg each at approximately 2-minute intervals. Then, PO 50 mg q6h beginning 15 minutes after the last IV dose; continue for 48 hours.
Condition: Late treatment of MI
Dose: PO 100 mg b.i.d. Continue for 1-3 months.
Adjustment of Dosage |
Kidney disease: None
Liver disease: None.
Elderly: None
Pediatric: Safety and efficacy have not been established.
Food and Drug Interactions |
Food: No restrictions.
Pregnancy: Category C.
Lactation: Appears in breast milk. Potentially toxic to infant. Wait at least 3-4 hours after dose before breastfeeding. Considered compatible by American Academy of Pediatrics. Observe infant for bradycardia, hypotension.
Contraindications: Cardiogenic shock, asthma, CHF unless it is secondary to tachyarrhythmia heatable with a β blocker, sinus bradycardia and AV block greater than first degree, severe COPD.
Warnings / Precautions |
> Use with caution in patients with diabetes, kidney disease, liver disease, COPD, peripheral vascular disease.
> Do not stop drug abruptly as this may precipitate arrhythmias, angina, MI or cause rebound hypertension. If necessary to discontinue, taper as follows: Reduce dose and reassess after 1-2 weeks. If status is unchanged, reduce by another 50% and reassess after 1-2 weeks.
> Drug may mask symptoms of hyperthyroidism, mainly tachycardia.
> Drug may exacerbate symptoms of arterial insufficiency in patients with peripheral or mesenteric vascular disease.
Clinically Important Drug Interactions |
> Drugs that increase effects/toxicity of β blockers: reserpine, bretylium, calcium channel blockers.
> Dmgs that decrease effects/toxicity of β blockers: aluminum salts, calcium salts, cholestyramine, barbiturates, NSAIDs, rifampin.
Adverse Reactions |
> Common: fatigue, dizziness.
> Serious: symptomatic bradycardia, CHF, worsened AV block, hypotension, depression bone marrow, depression, lupus-like condition, bronchospasm, Peyronie’s disease, hepatitis.
Parameters to Monitor |
> Liver enzymes, serum BUN and creatinine, CBC with differential and platelets.
> Pulse rate near end of dosing interval or before the next dose is taken. A reasonable target is 60-80 beats/min for resting apical ventricular rate. If severe bradycardia develops, consider treatment with glucagon, isoproterenol, IV atropine (1-3 mg in divided doses). If hypotension occurs despite correction of bradycardia, administer vasopressor (norephinephrine, dopamine or dobutamine).
> Symptoms of CHF. Digitalize patient and administer a diuretic or glucagon.
> Efficacy of treatment: decreased BP, decreased number and severity of anginal attacks, improvement in exercise tolerance. Confirm control of arrhythmias by ECG, apical pulse, BP, circulation in extremities and respiration. Monitor closely when changing dose.
> CNS effects. If patient experiences mental depression reduce dosage by 50%. The elderly are particularly sensitive to adverse CNS effects.
> Signs of bronchospasm. Stop therapy and administer large doses of β-adreneigic bronchodilator, eg, albuterol, terbutaline, or aminophylline.
> Signs of cold extremities. If severe, stop drug. Consider β blocker with sympathomimetic properties.
Advice to Patient |
> Avoid driving and other activities requiring mental alertness or that are potentially dangerous until response to drug is known.
> Dress warmly in winter and avoid prolonged exposure to cold as drug may cause increased sensitivity to cold.
> Avoid drinks that contain xanthines (caffeine, theophylline, theobromine) including colas, tea, and chocolate because they may counteract the effect of drug.
> Restrict dietary sodium to avoid volume expansion.
> Drug may blunt response to usual rise in BP and chest pain under stressful conditions such as vigorous exercise and fever.
Further Useful Info |
> Stopping a β blocker before surgery is controversial. Some advocate discontinuing the drug 48 hours before surgery; others recommend withdrawal for a considerably longer time. Notify anesthesiologist that patient has been on β blocker.
> β blockers are first-line treatments for hypertension, particularly in patients with the following conditions: previous MI, ischemic heart disease, aneurysm, atrioventricular arrhythmias, migraine. These are drugs of first choice for chronic stable angina, used in conjunction with nitroglycerin.
> Many studies indicate benefit from administration of a β blocker following an MI.
> β Blockers are considered to be first-line drugs for prophylaxis of migraine headache in patients who have two or more attacks per month.



