Itraconazole is an antifungal medication used to treat a number of fungal infections. This includes aspergillosis, blastomycosis, coccidioidomycosis, histoplasmosis, and paracoccidioidomycosis. It may be given by mouth or intravenously.
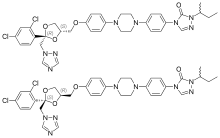
Molecular Structure |
Class of Drug |
Antifungal agent.
Mechanism of Action |
Inhibits fungal cytochrome P450 synthesis of ergosterol, resulting in decreased cell wall integrity and leakage of essential cellular components.
Susceptible organisms in vivo: Not for cryptococcosis (fluconazole is preferred). Blastomyces dermatidis, Candida, Histoplasma, Aspergillus flavus, Coccidioides immitis Sporotrichosis.
Indications / Dosage / Route |
Routes of Administration: Oral only.
Condition: Blastomycosis or histoplasmosis
Dose: Adults: 200 mg once daily. If there is no improvement or the disease is progressive, the dose may be increased in 100-mg increments. Maximum: 400 mg/d.
Children: 3-16 years: 100 mg/d.
Condition: Aspergillosis
Dose: Adults: 400 mg daily.
Condition: Life-threatening infections
Dose: Adults: 200 mg t.i.d. for the first 3 days.
Condition: Onychomycosis
Dose: Adults: 200 mg once a day for 12 consecutive weeks.
Condition: Oral solution: oropharyngeal candidiasis
Dose: Adults: 200 mg/d for 1-2 weeks.
Condition: Oral solution: esophageal candidiasis
Dose: Adults: 100 mg/d, minimum 3 weeks.
Adjustment of Dosage |
Kidney disease: None.
Liver disease: None.
Elderly: None
Pediatric: Safety and efficacy have not been established in children <3 years.
Food and Drug Interactions |
Food: Should be taken with food.
Pregnancy: Category C.
Lactation: Appears in breast milk. Avoid breastfeeding.
Contraindications: Hypersensitivity to itraconazole and other azole antifungals, coadministration of astemizole, triazolam, midazolam, treatment of onchomycosis during pregnancy.
Warnings / Precautions |
> Review drugs that patient is currently taking to avoid possible dangerous drug drug interactions.
Clinically Important Drug Interactions |
> Itraconazole increases effects/toxicity of the following: astemizole, calcium blockers, cisapride, cyclosporine, digoxin, midazo¬lam, sulfonylureas, tacrolimus, triazolam, warfarin.
> The following drugs decrease effects/toxicity of the following: itraconzole: isoniazid, phenytoin, rifampin, phenobarbital.
Adverse Reactions |
> Common: nausea, vomiting, diarrhea, abdominal pain, rash.
> Serious: hepatotoxicity (rare), exfoliative skin disorders (rare).
Parameters to Monitor |
> Signs and symptoms of liver toxicity, particularly in patients receiving treatment longer than 1 month.
> Symptoms indicating reactivation of blastomycosis: rales, chest pain, cough, fever, rash, SOB, weight loss.
> Symptoms indicating reactivation of histoplasmosis: Chest pain, generalized pain, rales, SOB, weight loss.
Advice to Patient |
> Report symptoms of possible liver dysfunction: jaundice, anorexia, dark urine, pale stools, nausea, vomiting.
> Avoid driving and other activities requiring mental alertness or that are potentially dangerous until response to drug is known.
> Avoid alcohol.
> To minimize possible photosensitivity reaction, apply adequate sunscreen and use proper covering when exposed to strong sunlight.
Further Useful Info |
> Itraconazole is not used for cryptococcosis (fluconazole is preferred). It is a broad-spectrum antifungal agent and covers Aspergillus species.
> For severe infections, amphotericin B is preferred.
> Itraconazole is very effective against onycomycosis, Candida infections, Blastomyces, Histoplasma, coccidiomycosis, aspergillosis, and sporotrichosis. It is effective for CNS infections. In general, amphotericin B is used acutely, then itraconazole is given as long term therapy.


