Betamethasone is a steroid medication. It is used for a number of diseases including rheumatic disorders such as rheumatoid arthritis and systemic lupus erythematosus, skin diseases such as dermatitis and psoriasis, allergic conditions such as asthma and angioedema, preterm labor to speed the development of the baby’s lungs, Crohn’s disease, cancers such as leukemia, and along with fludrocortisone for adrenocortical insufficiency.
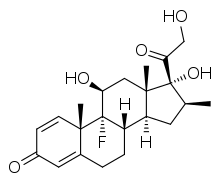
Molecular Structure |
Class of Drug |
Topical and systemic antiinflammatory glucocorticoid.
Mechanism of Action |
Inhibits migration of polymorphonuclear leukocytes; stabilizes lysomal membranes; inhibits production of products of arachidonic acid cascade.
Indications / Dosage / Route |
Routes of Administration: IM, topical, intraarticular, intrabursal, intradermal. Dosages of corticosteroids are variable. These should be individualized according to the disease being treated and the response of the patient.
Condition: Adrenal insufficiency
Dose: Adults: IM 0.5 mg/d.
Condition: Bursitis, peritendinitis, tenosynovitis
Dose: Adults: Intrabursal: 3 mg (1 mL).
Condition: Rheumatoid arthritis and osteoarthritis
Dose: Adults: Intraarticular: 0.75-6 mg (0.25-2 mL).
Condition: Acute gouty arthritis
Dose: Adults: Intraarticular 1.5-3 mg (0.5-1 mL).
Condition: Dermatologic conditions
Dose: Adults Intradermal: 0.2 mL/cm2, not to exceed 1 mL/wk.
Condition: Corticosteroid-responsive dermatoses
Dose: Children: Apply thin layer to affected area once or twice a day
Adjustment of Dosage |
Kidney disease: None.
Liver disease: None.
Elderly: None.
Pediatric: Systemic use: Children on long-term therapy must be monitored carefully for growth and development. Topical use: Safety and efficacy have not been established in children <12.
Food and Drug Interactions |
Food: Not applicable.
Pregnancy: Category C.
Lactation: No data available. Best to avoid.
Contraindications: Systemic use: fungal, viral, or bacterial infections, Cushing’s syndrome. Topical use: hypersensitivity to corticosteroids, markedly impaired circulation, occlusive dressing if primary skin infection is present, monotherapy in primary bacterial infections, eg, impetigo, cellulitis, rosacea, ophthalmic use, plaque psoriasis (widespread).
Warnings / Precautions |
> Use with caution in patients with the following conditions: diabetes mellitus, cardiovascular disease, hypertension, throm-bophlebitis, renal or hepatic insufficiency. Topical agent: Use with caution in patients with primary skin infections and those receiving other immunosuppressant drugs.
> Skin test patient for tuberculosis before beginning treatment if patient is at high risk.
> For long-term treatment consider alternative-day dosing; however, if the disease flares, may need to return to initial daily dose.
> Observe neonates for signs of adrenal insufficiency if mother has taken steroids during pregnancy.
> Tapering is always required when administration of a steroid is stopped. A variety of procedures for tapering after long-term therapy have been suggested. For example, taper dose by 5 mg/ wk until 10 mg/d is reached. Then 2.5 mg/wk until therapy is discontinued or lowest dosage giving relief is reached. Longer tapering periods may be required for some patients. Adrenal insufficiency may persist for up to 1 year.
> Attempt dose reduction periodically to determine if disease can be controlled at a lower dose. When every-other-day therapy is initiated, twice the daily dose should be administered on alternate days in the morning.
> Check whether patient is allergic to tartrazine which is present in some of these drugs.
Clinically Important Drug Interactions |
> Systemic
> Drugs that increase effects/toxicity of corticosteroids: broad spectrum antibiotics, anticholinergics, oral contraceptives, cyclosporine, loop diuretics, thiazide diuretics, NSAIDs, tricyclic antidepressants.
> Drags that decrease effects/toxicity of corticosteroids: barbiturates, cholestyramine, ketoconazole, phenytoin, rifampin.
> Corticosteroids increase effects/toxicity of following drugs: digitalis glycosides, neuromuscular blocking drugs.
> Corticosteroids decrease effects of vaccines, toxoids.
> Topical: None.
Adverse Reactions |
> Common: dyspepsia, appetite stimulation, insomnia, anxiety, fluid retension, cushinoid facies.
> Serious: Cushing-like syndrome, adrenocortical insufficiency, muscle wasting, osteoporosis, immunosuppression with increased susceptibility to infection, potassium loss, glaucoma, cataracts (nuclear, posterior, subcapsular), hyperglycemia, hypercorticism, peptic ulcer, psychosis, insomnia, skin atrophy, thrombosis, seizures, angioneuritic edema. Children: Growth suppression, pseudotumor cerebri (reversible papilledema, visual loss, nerve paralysis [abducens or oculomotor]), vascular bone necrosis, pancreatitis.
> Topical: Common: itching, burning, skin dryness, erythema, folliculitis, hypertrichosis, allergic contact dermatitis, skin maceration, secondary infection, striae, miliaria, skin atrophy. Serious: HPA axis suppression, Cushing’s syndrome.
Further Useful Info |
Corticoid treatment remains challenging for clinicians due to commonly occurring short-term and long-term side effects. With chronic use, adrenal suppression may persist for up to 1 year. The agents produce accelerated bone resorption as well as decreased bone formation, resulting in overall bone loss with chronic use. Ongoing monitoring is suggested and treatment with bisphosphonates or calcitonin is suggested when decreased bone mineral density occurs.


