Amikacin is an antibiotic used for a number of bacterial infections. This includes joint infections, intraabdominal infections, meningitis, pneumonia, sepsis, and urinary tract infections. It is also used for the treatment of multidrug-resistant tuberculosis
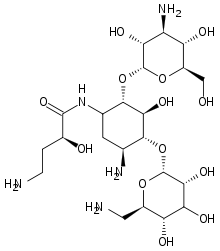
Molecular Structure |
Class of Drug |
Antibiotic, Aminoglycoside.
Mechanism of Action |
Binds to ribosomal units in bacteria, inhibits protein synthesis.
Susceptible organisms in vivo: Staphylococci (penicillinase and nonpenicillinase), Staphylococcus epidermidis, Acinetobacter sp, Citrobacter sp, Enterobacter sp, Escherichia coli, Klebsiella sp, Proteus sp, Providencia sp, Pseudomonas sp, Serratia sp.
Indications / Dosage / Route |
Routes of Administration: IM, IV.
Condition: Bacterial septicemia (including neonatal sepsis); serious infections of the respiratory tract, bones, joints, skin, soft tissue, and CNS (eg, meningitis); burns; serious complicated infections of the urinary tract
Dose: Adults, children, older infants: 15 mg/kg in 2-3 divided doses, 7-10 days. Maximum: 15 mg/kg/d
Condition: Uncomplicated UTIs
Dose: Adults: 250 mg b.i.d.
Newborns: loading dose of 10 mg/kg, then 7.5 mg/kg ql2h.
Adjustment of Dosage |
Kidney disease: initial: 7.5 mg/kg (loading dose); maintenance: divide normal recommended dose by patient’s serum creatinine level, administer calculated dose ql2h.
Food and Drug Interactions |
Food: No restrictions.
Pregnancy: Category D.
Lactation: Appears in breast milk in small amounts. Potentially toxic to infant. Best to avoid.
Contraindications: Hypersensitivity to aminoglycoside antibiotics.
Warnings / Precautions |
> Use with caution in patients with the following conditions: renal disease, neuromuscular disorders (eg, myasthenia gravis, parkinsonism), hearing disorders.
> Do not combine this drug with any other drug in the same IV bag.
Clinically Important Drug Interactions |
> Drugs that decrease effects/toxicity of aminoglycosides: penicillins (high dose), cephalosporins.
> Drugs that increase effects/toxicity of aminoglycosides: loop diuretics, amphotericin B, enflurane, vancomycin, NSAIDs.
Adverse Reactions |
> Common: None.
> Serious: Renal toxicity, ototoxicity, neuromuscular paralysis, respiratory depression (infants), superinfection.
Parameters to Monitor |
> Determine peak and trough serum levels 48 hours after beginning therapy and every 3-4 days thereafter as well as after changing doses.
> Monitor patient for ototoxicity: tinnitus, vertigo, hearing loss. The drug should be stopped if tinnitus occurs. Limit administration to 7-10 days to decrease the risk of ototoxicity.
> Monitor patient’s renal function periodically. If serum creatinine increases by more than 50% over baseline value, it may be advisable to discontinue drug treatment and use a less nephrotoxic agent, eg, a quinolone or cephalosporin.
> Efficacy of drug action: If there is no response in 3-7 days, reculture and consider another drug.
> Monitor neuromuscular function when administering the drug IV. Too rapid administration may cause paralysis and apnea. Have calcium gluconate or pyridostigmine available to reverse such an effect.
> Monitor patient’s neurologic status if the drug is given for hepatic encephalopathy.
> Monitor patient for signs and symptoms of allergic reaction.
Further Useful Info |
> Once daily dosing of amikacin has been advocated by some authors to increase efficacy and reduce toxicity.


